| Portal Hypertension Imaging Strategies
Author Brian Hashim MS4
Under construction
Clinical Considerations: When considering the patient with portal hypertension, it is helpful to consider the potential causes in terms of three categories, those being pre-sinusoidal, sinusoidal, and post-sinusoidal. With portal hypertension, both the severity of disease as well as its sequelae are varied. Thus, when considering what tests to order as well as imaging strategies, the physician must first assess the severity of the patient’s condition clinically and determine if it is feasible to await the results of blood or imaging studies. If a patient’s condition is severe (eg. bleeding esophageal varices), such studies should be put on hold until the patient becomes more stable.
Imaging Strategies: Given the patient is stable, the physician should first consider what is most suspicious of as the etiology for the patient’s portal hypertension. If one is suspicious of a clot, either MRI or CT with contrast may be considered, although ultrasound would give helpful data as well. Below is a table of the possible radiographic studies that may be used in the evaluation of portal hypertension as well as their strengths and limitations.
Table 1. Radiographic studies in evaluation of portal HTN
What Study? As an initial screening test, it seems Duplex-Doppler ultrasound is the best choice regardless of the considered etiology. This test provides insight into both the anatomy and physiology of the portal vascular system.
Why Duplex-Doppler Ultrasound? As mentioned above, this study provides information with respect to both the anatomy and physiology of the portal vascular system. Along with this strength, ultrasound is a safe, cheap, and non-invasive study. If findings from U/S are non-diagnostic or the study is low yield secondary to patient’s body habitus/bowel gas, the physician should consider further investigation with either CT scan w/ contrast or MRI.
Background to Disease: Portal hypertension is defined as an increased pressure within the portal vasculature secondary to either increased portal flow or, in most cases, increased resistance to flow. It should be sought in all patients with a suspicion of liver disease. Normal portal pressure is considered to be 5-10mmHg, with values >10mmHg defining portal hypertension. Alone, portal hypertension is asymptomatic. Patients present with signs/symptoms of portal hypertension once complications such as esophageal varices develop. As mentioned above, the etiology of portal hypertension can be divided into three main groups, those being pre-sinusoidal, sinusoidal, and post-sinusoidal. A table of the different causes may be seen below. In industrialized nations, cirrhosis is by far the most common cause. Over time, as the body remains exposed to high portal pressures, blood flow seeks the path of least resistance, forming portal-systemic venous collaterals. The most dangerous complication associated with the development of such collaterals if bleeding esophageal varices.
Table 2. Causes of Portal HTN
When to Order? In a patient whom is hemodynamically stable, one might consider Duplex-Doppler U/S to assess the degree of compromise of blood flow in the portal vasculature whenever there is a suspicion of liver failure. Patients presenting with bleeding esophageal varices by definition have portal hypertension, and given the mortality associated with this complication, should undergo treatment for the bleeding varices rather than have any radiographic studies performed.
How to Order? There is no preparation necessary prior to undergoing Duplex-Doppler U/S for the assessment of portal hypertension. At the time of ordering an U/S, one should include any symptoms that the patient may be exhibiting as well as the pertinent history. One should be sure to include the intent of the imaging study, such as “the evaluation for possible portal hypertension”. If CT scan w/ contrast is to be ordered, the patient’s allergies should be reviewed to ensure no dye allergies are present. The patient’s BUN and Creatinine should also be assessed so as to limit the occurrence of acute renal failure secondary to contrast. If MRI is to be obtained, one should ensure that the patient will be able to remain still for the length of the study and also ensure that the patient has no metallic implanted devices (eg. Pacemaker).
Preparing the Patient: For the hemodynamically stable non-hospitalized patient, any of the above mentioned studies may be performed with the patient returning to work or home the same day. Patients should be reminded that all of the studies are non-invasive and provide same day results. So as to limit anxiety for the patient, time should be allotted to answer any and all questions regarding the imaging modality of choice. For patients with a history of claustrophobia who are to undergo MRI, premedication should be considered.
Clinical Red Flags: Any patient presenting with bleeding esophageal varices should have the bleeding varices treated. Imaging studies to diagnose portal hypertension are contraindicated in such cases.
References: Texts: Schwartz’s Principles of Surgery, 8th edition 2005 Merck Manual, 17th edition, 1999, Centennial edition Griffith’s 5-Minute Clinical Consult, 14th edition, 2006 Web: eMedicine-Portal hypertension |
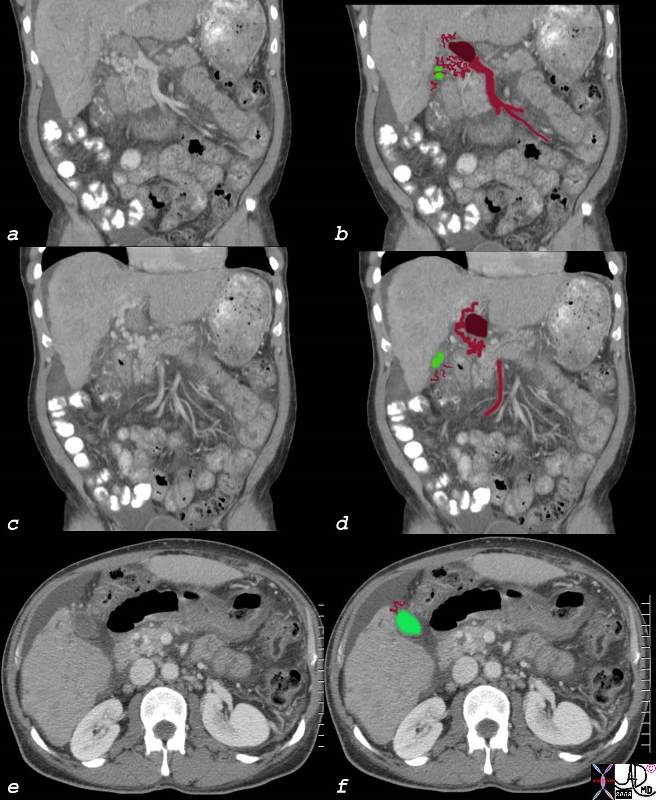
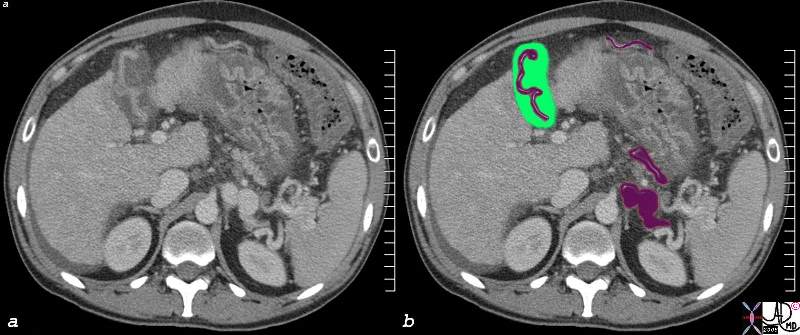 Gallbladder Varicosity
Gallbladder Varicosity