Katie Dam MS4
- For some reason ACR Criteria are only showing up in the google docs sent
- At the end are also the symptom driven ACR Appropriateness criteria that we have to add in our categories We may call this program “What next?”
- At the end is the modality oriented headings that they did not do
-
Word Definition Image TCV Link ACR Appropriateness Criteria Cerebral Abscess A cerebral abscess is an infectious accumulation of pus located within the brain tissue. It is typically caused by an infectious organism like bacteria, often originating from a nearby infection or through blood-borne spread from another part of the body. It is characterized by symptoms such as headache, fever, neurologic deficits (such as weakness or altered mental status), and signs of increased intracranial pressure. This results in imaging findings of focal, round lesions with ring enhancement seen on MRI and sometimes CT. 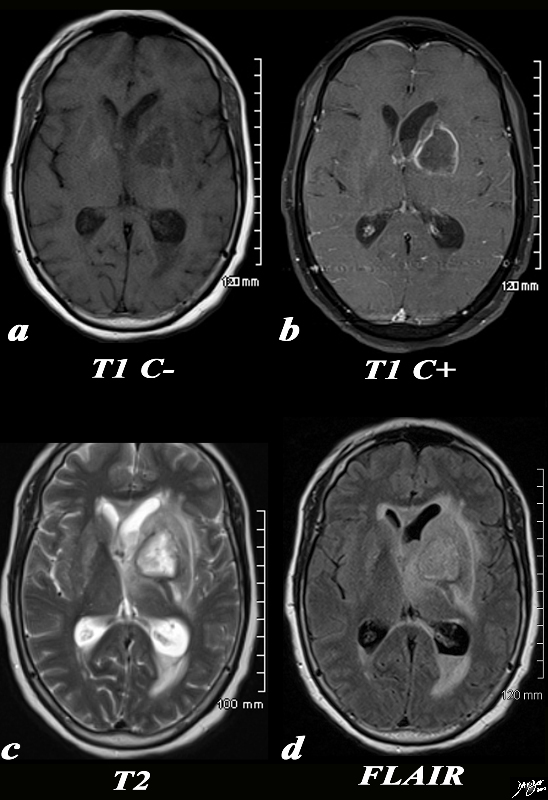
https://www.thecommonvein.net/media/89054c.8s.jpg
Brain Abscess Paraspinal Abscess A paraspinal abscess is an infectious accumulation of pus located within the paraspinal soft tissues adjacent to the spinal column. It is typically caused by an infectious organism like bacteria, often originating from nearby infections like vertebral osteomyelitis, or as a complication of spinal surgery or trauma. It is characterized by symptoms such as localized pain, swelling, tenderness, fever, and occasionally neurologic deficits if the abscess compresses on spinal nerves. This results in imaging findings of fluid collections or abscess formations adjacent to the spine with surrounding tissue inflammation, seen on MRI or CT. 
https://radiopaedia.org/cases/epidural-and-paraspinal-abscesses?lang=us
Age Related Changes Age-related changes of the brain are structural and functional alterations that occur as a natural consequence of aging within the brain. They are generally caused by a combination of factors, including neuronal loss, reduced blood flow, accumulation of cellular waste productions, and changes in neurotransmitter levels. They may be characterized by a decline in cognitive functions such as memory, processing speed, and executive function. Imaging studies like MRI may reveal generalized brain atrophy (decrease in brain volume), particularly in the frontal and temporal lobes (prefrontal cortex and hippocampus, respectively), as well as changes in white matter integrity such as increased hyperintensities on T2-weighted imaging. However, these changes are considered within the normal spectrum of aging and not indicative of pathological conditions in most cases. 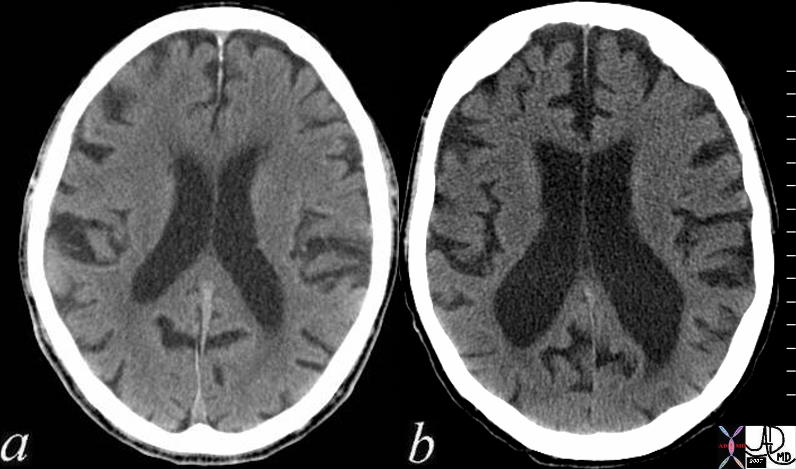
https://thecommonvein.net/media/72179c01.jpg
Growth and Aging Cerebral Aneurysm A cerebral aneurysm is a structural abnormality of blood vessels, typically found in arteries within the brain. It is typically caused by a weakened or bulging area in the wall of a cerebral blood vessel, the formation of which can be a result of several factors including genetic predisposition, high blood pressure, atherosclerosis, trauma, or certain medical conditions. These are often asymptomatic until they rupture, which can lead to a sudden and severe headache, neck stiffness, nausea, vomiting, and/or neurological deficits such as vision changes, weakness, or seizures. Imaging with cerebral angiography, CT angiography (CTA), or magnetic resonance angiography (MRA) typically reveals a localized dilation or bulging of the affected cerebral artery. 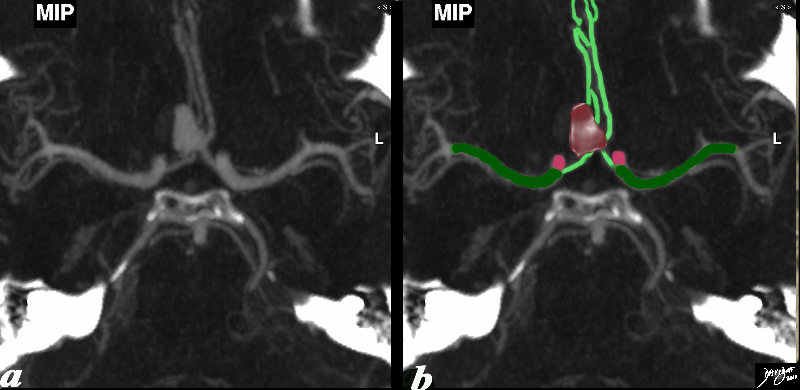
https://www.thecommonvein.net/media/92577c01b8.jpg
Cerebral Aneurysm Spinal Cord Compression A spinal cord compression refers to the pathological condition where there is pressure exerted on the spinal cord within the vertebral canal. This is often caused by encroachment or narrowing of the spinal canal, which can be a result of various factors such as herniated discs, spinal tumors (benign or malignant), spinal stenosis, trauma, infections, or degenerative changes in the spine. Symptoms may include localized or radiating pain, weakness, numbness, tingling sensations, and in severe cases, loss of bowel/bladder control and paralysis. Imaging studies like MRI or CT will show the compression of the spinal cord itself as well as the cause of compression in most cases; imaging could demonstrate spinal cord compression by showing narrowing of the spinal canal, presence of tumors, herniated discs, or other structural abnormalities impacting the spinal cord.  https://radiopaedia.org/cases/cervical-canal-stenosis-with-cord-compression?lang=us
https://radiopaedia.org/cases/cervical-canal-stenosis-with-cord-compression?lang=usDementia (Atrophy) Dementia is a degenerative neurological condition that occurs primarily within the cognitive functions of the brain. It can be caused by various underlying conditions, the most common being Alzheimer’s disease. Other causes include vascular dementia, Lewy body dementia, frontotemporal dementia, and mixed dementia (a combination of different types). It is characterized by a decline in cognitive function severe enough to interfere with daily life and activities, symptoms of which include memory loss, difficulties with language, impaired judgment, impaired reasoning, and/or changes in mood or behavior. Progression of dementia leads to a gradual decline in cognitive abilities affecting multiple domains. Imaging findings might include brain atrophy and changes in specific brain regions seen on MRI, however diagnosis is often based on clinical assessment, medical history, and cognitive testing rather than solely on imaging findings. 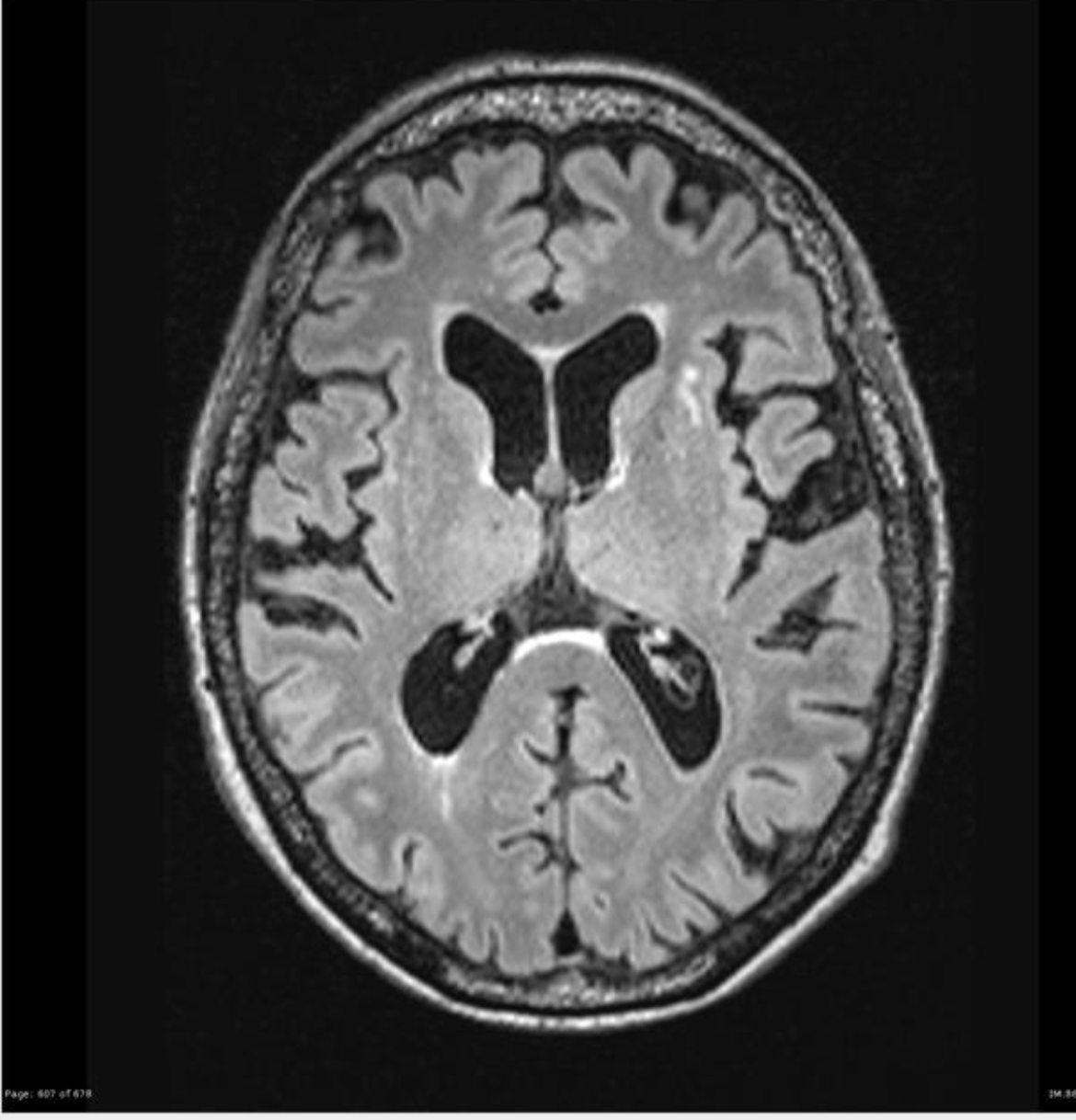 https://radiopaedia.org/cases/alzheimer-disease-1?lang=us
https://radiopaedia.org/cases/alzheimer-disease-1?lang=usDiffuse Axonal Injury Diffuse axonal injury is a traumatic structural abnormality involving widespread damage to the brain’s white matter tracts, which can occur throughout various regions of the brain where axonal shearing takes place. This is caused by rapid acceleration or deceleration forces, which is typically seen in cases of traumatic events leading to severe head injury, such as car accidents, falls, or severe shaking that can cause rotational forces that shear and damage the brain’s axons. Diffuse axonal injury can present with varying degrees of consciousness, ranging from mild confusion to coma. Symptoms can include prolonged unconsciousness, cognitive deficits, physical impairments, and behavioral changes. Imaging with MRI may reveal multiple small punctate hemorrhagic lesions involving the white matter tracts, but the diagnosis is often based on clinical history, physical examination, and consideration of the mechanism of injury rather than solely on imaging findings. 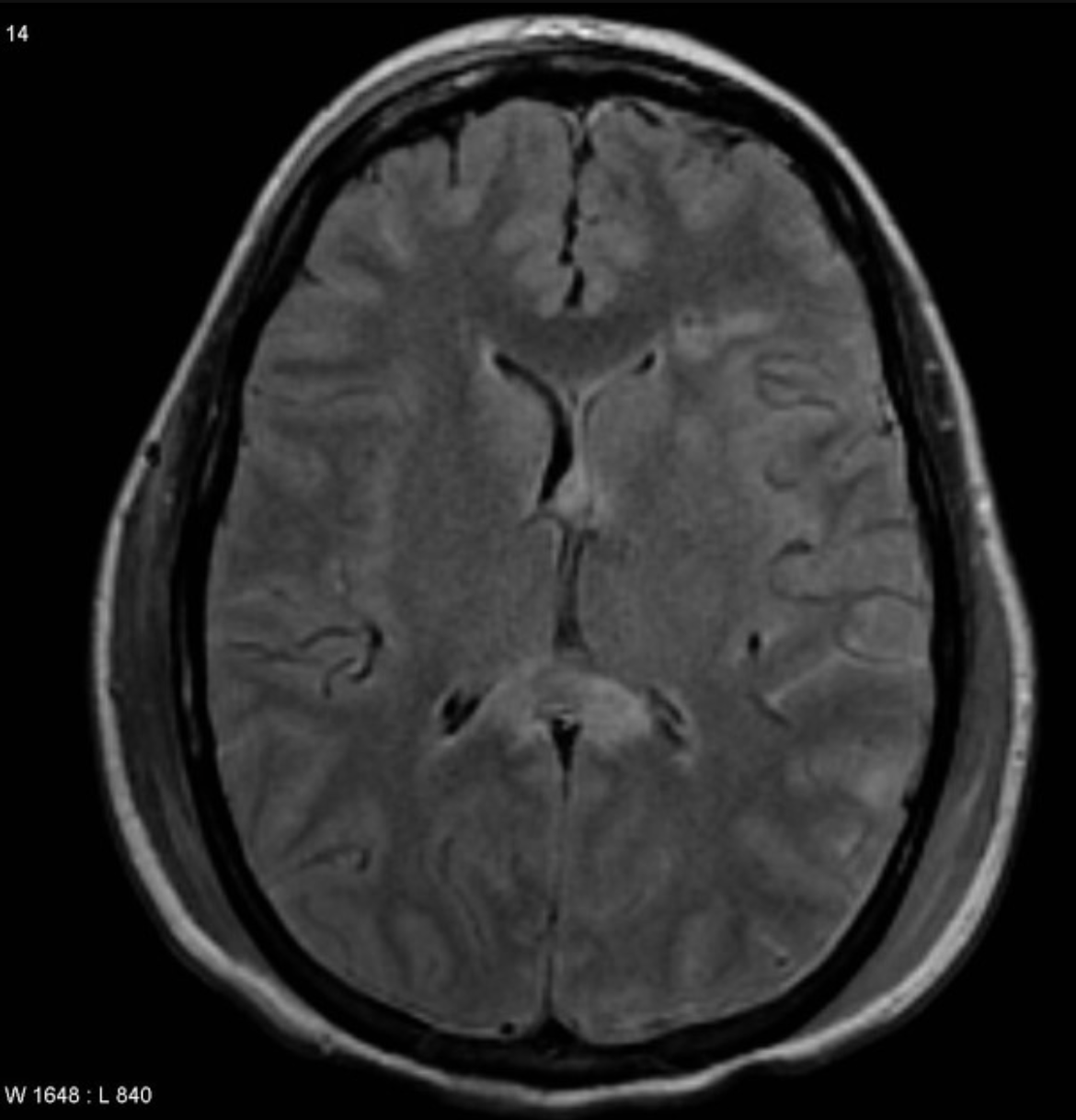 https://radiopaedia.org/cases/diffuse-axonal-injury?lang=us
https://radiopaedia.org/cases/diffuse-axonal-injury?lang=usDiffuse Axonal Injury Subdural Hematoma A subdural hematoma is a traumatic or nontraumatic accumulation of blood between the dura mater (outermost covering) and the arachnoid membrane (middle layer) of the brain. This typically occurs as a result of head trauma/injury that causes tearing of the bridging veins, which leads to bleeding into the potential space between the dura and the arachnoid membranes. This can also occur spontaneously due to conditions such as anticoagulation therapy, bleeding disorders, or elderly individuals with cerebral atrophy. Symptoms might not appear immediately after the injury, but can include headache, confusion, dizziness, nausea, vomiting, seizures, focal neurological deficits, or altered consciousness. Severe cases can lead to increased intracranial pressure and rapid deterioration. Imaging with CT or MRI will show a crescent-shaped collection of blood between the brain and its coverings, often exerting pressure on the brain tissue. 
https://thecommonvein.net/media/70000.800.jpg
Subdural Hematoma Epidural Hematoma An epidural hematoma is a traumatic accumulation of blood between the dura mater (outermost covering of the brain) and the inner surface of the skull. This typically occurs as a result of head trauma/injury that causes rupture of the middle meningeal artery, which leads to bleeding into the space between the skull and the dura. The bleeding can then rapidly increase, leading to formation of a hematoma. This often presents with a lucid interval after the initial trauma, followed by the rapid onset of symptoms such as severe headache, nausea, vomiting, dizziness, confusion, or loss of consciousness due to the increasing pressure on the brain. Imaging with CT will show a lens-shaped or biconvex collection of blood between the brain and the skull that is typically localized and does not cross the suture lines of the skull. 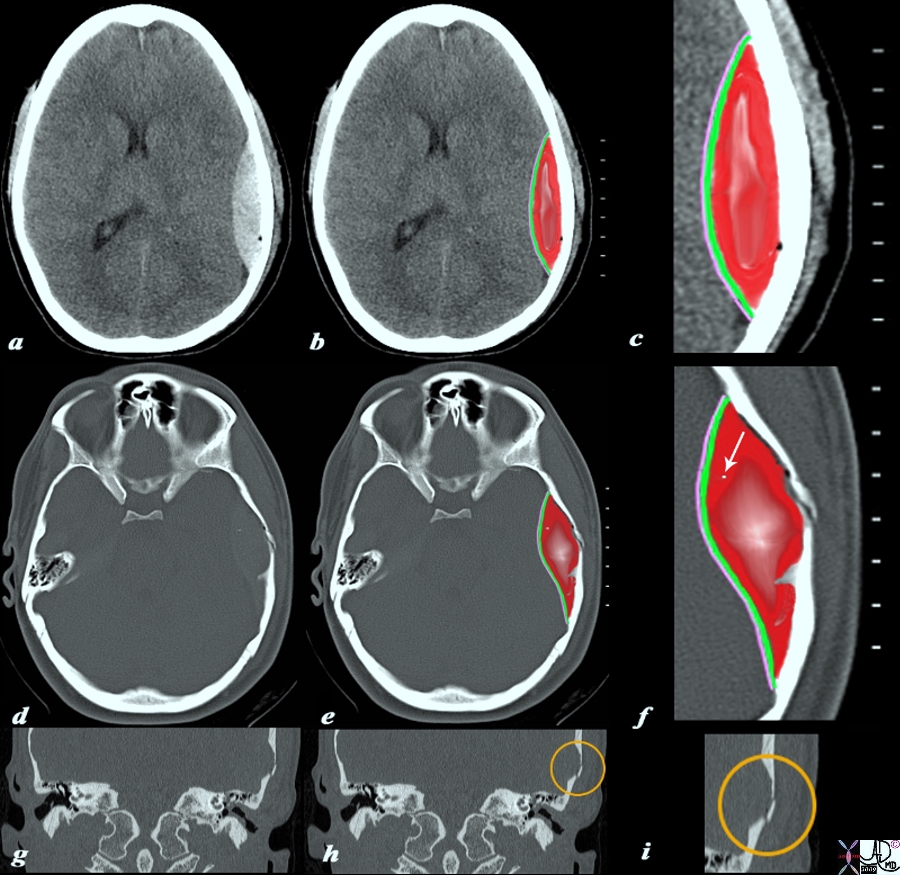
https://www.thecommonvein.net/fractures/wp-content/uploads/2020/10/98056c04.9s.jpg
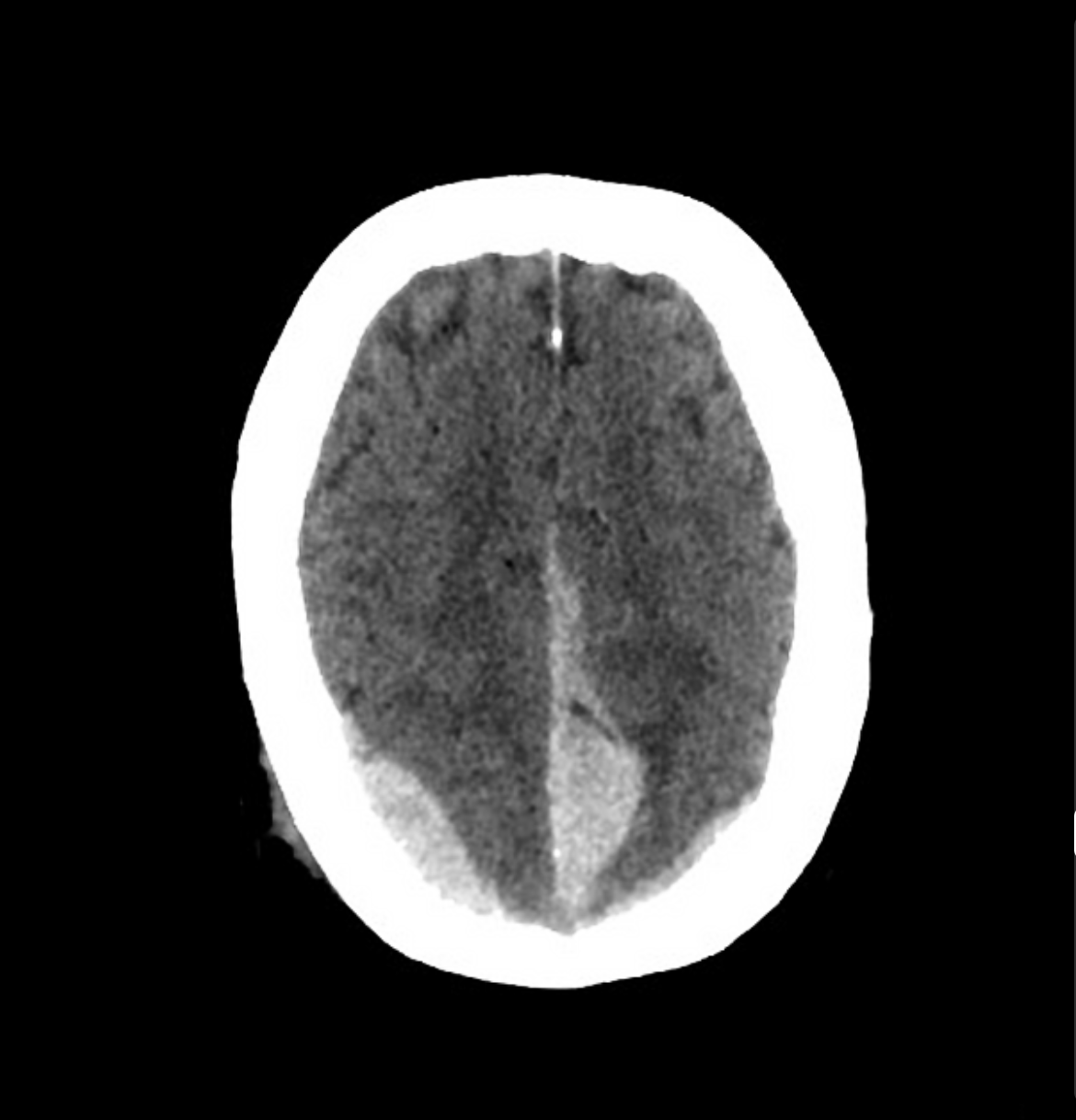
Epidural Hematoma Intracerebral hemorrhage An intracerebral hemorrhage is an occurrence of bleeding within the brain tissue itself, leading to the formation of a hematoma. This is typically caused by the rupture of a blood vessel (artery or vein) within the brain, often due to conditions such as hypertension, cerebral amyloid angiopathy, arteriovenous malformations, trauma, or aneurysm rupture. Symptoms can vary depending on the location and size of the bleed, but often include sudden onset of severe headache, focal neurological deficits (such as unilateral weakness, speech difficulties, vision changes), altered mental status, nausea, vomiting, and seizures. Imaging with CT will show a hyperdense lesion within the brain parenchyma, indicating the presence of bleeding. MRI sequences sensitive to blood products will also indicate the presence of bleeding within the brain parenchyma, appearing as areas of high signal intensity. 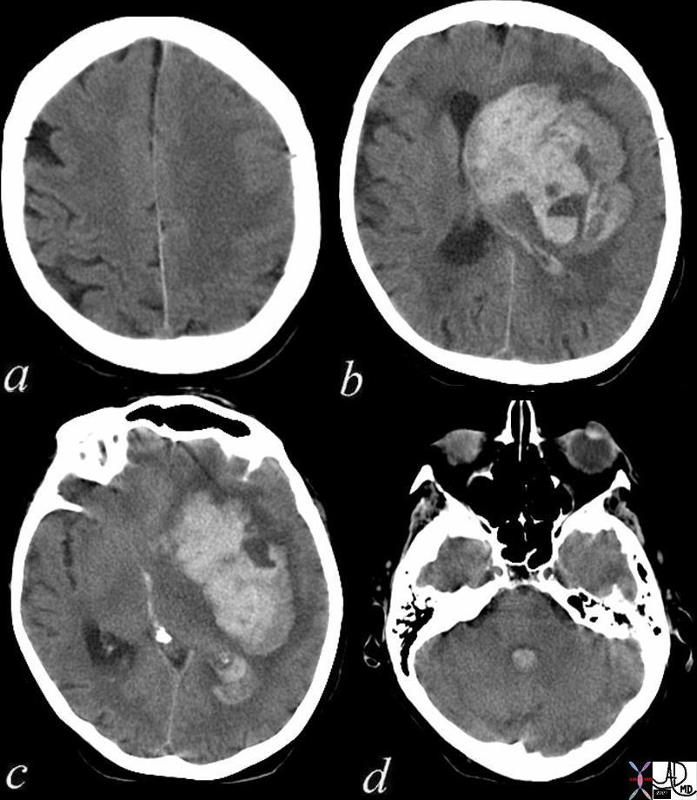 https://www.thecommonvein.net/expertadviceinradiology/wp-content/uploads/2017/12/72143c01.jpg
https://www.thecommonvein.net/expertadviceinradiology/wp-content/uploads/2017/12/72143c01.jpgIntracerebral Hemorrhage Isodense Subdural Hematomas Isodense subdural hematomas refer to a specific type of subdural hematoma that appears on CT to have a similar density to surrounding brain tissue. Similar to other subdural hematomas, these also are located between the dura mater (outermost covering) and the arachnoid membrane (middle layer) of the brain, within the intracranial space. Isodense subdural hematomas are usually caused by venous bleeding, and may be associated with a slower rate of bleeding compared to other subdural hematomas. Due to the nature of having similar density to surrounding brain tissue on CT, isodense subdural hematomas can be challenging to detect on initial imaging. Confirming their presence may require careful scrutiny with additional imaging sequences or follow-up scans, as blood products will be reabsorbed with time. The isodense subdural hematomas can then start showing increased prominence as the density changes, becoming more conspicuous on subsequent scans or MRI sequences. Image #17354.8? “Bifrontal Isodense Subdural hematomas”
https://radiopaedia.org/cases/isodense-subdural-haematoma?lang=us
Subdural Hematoma Subarachnoid Hemorrhage Subarachnoid hemorrhage is a type of bleeding that occurs in the subarachnoid space, which is the area between the arachnoid membrane (middle layer) and the pia mater (inner layer) surrounding the brain. This is most commonly caused by the rupture of an intracranial aneurysm, though there can be other causes such as arteriovenous malformations (AVMs), head trauma, or bleeding disorders. This often presents with a sudden, severe headache (described as “the worst headache of my life”), nausea, vomiting, altered mental status, neck stiffness (due to irritation of the meninges), and sometimes loss of consciousness or seizures. Imaging with CT will show blood in the subarachnoid space appearing as hyperdensity, which is commonly seen in the basal cisterns or sulci around the brain. A lumbar puncture can confirm the presence of blood in the cerebrospinal fluid. Immediate medical attention and specialized care are essential due to the potentially life-threatening nature of this condition. 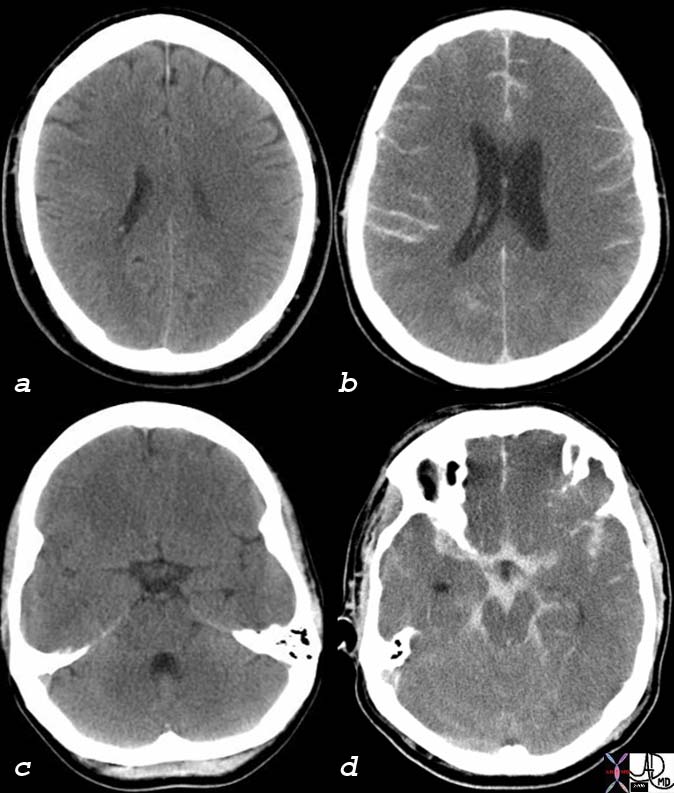
https://www.thecommonvein.net/media/76059c01_1.jpg
Subarachnoid Hemorrhage Hematomas of Different Ages in Nonaccidental Trauma Hematomas of different ages in nonaccidental trauma refer to various stages of bleeding or collections of blood at different stages of evolution found in cases of suspected or confirm child abuse or nonaccidental injury. Depending on the nature of the trauma, hematomas can be found in different locations within or around the head or brain, and they occur due to repeated or severe traumatic events inflicted upon the victim, often in cases of physical abuse or intentional harm. Hematomas of different ages may present as varying stages of healing, and can include acute/recent hematomas with fresh bleeding, subacute hematomas showing signs of organization or partial resolution, and chronic hematomas exhibiting signs of breakdown and reabsorption of blood products. Therefore, having this spectrum of hematomas at different stages suggests repeated trauma over time. On imaging with CT or MRI, findings might reveal multiple hematomas in various stages of evolution, possibly located in different areas of the head/brain.
- Acute/recent hematomas with fresh bleeding will appear hyperdense (bright) on CT imaging due to the high attenuation of fresh blood, often with sharper and more well-defined borders. Active bleeding may show contrast enhancement within the hematoma due to ongoing leakage or accumulation of blood products. A phenomenon known as the “swirl sign” or the “blend sign” might also be seen, indicating active bleeding with mixed densities within the hematoma. On MRI, acute hematomas will appear hyperintense on T1-weighted images and hypointense on T2-weighted images. Acute bleeds often have a more pronounced mass effect with compression of adjacent structures and significant surrounding edema due to the sudden accumulation of blood.
- As the bleed ages, chronic/old hematomas will become more isodense and more diffuse with less distinct borders on CT imaging, due to the natural breakdown and reabsorption of blood products over time. On MRI, chronic hematomas are isointense to hypointense on T1-weighted images, and hyperintense on T2-weighted images. Older bleeds might have less mass effect and reduced edema as the blood begins to break down and the body absorbs it.
- Subacute hematomas may show varying densities on imaging, with the center becoming less dense due to clot retraction and breakdown products.
The presence of hematomas in various stages of healing may raise suspicion for nonaccidental trauma, prompting further investigation and evaluation by healthcare professionals and child protection services.
No TCV images 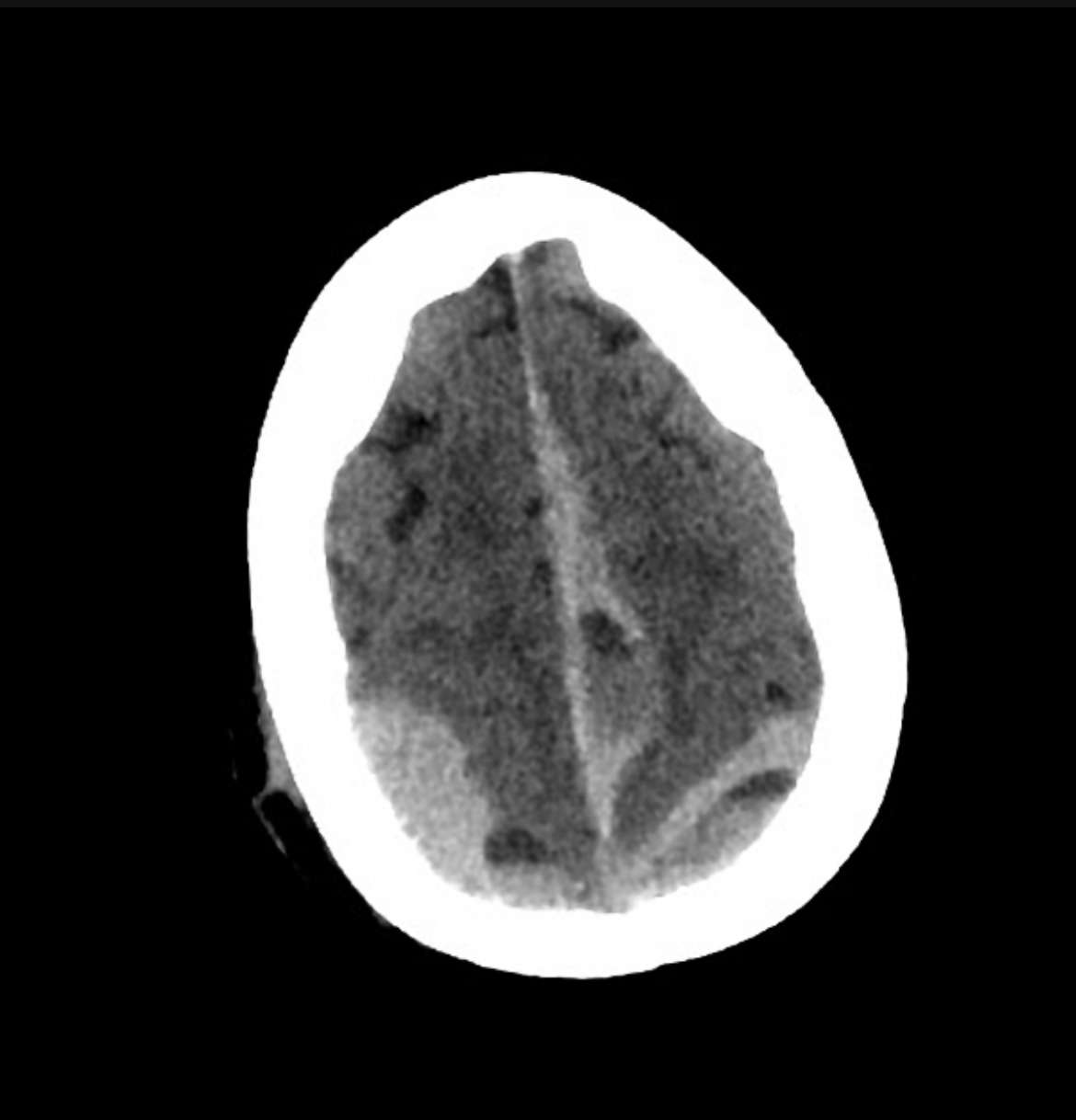
^four hours later
https://radiopaedia.org/cases/subdural-haematoma-three-ages-of-blood?lang=us
Intracranial Hemorrhage Cerebral Herniation A cerebral herniation is an abnormal displacement or shifting of brain tissue from its usual position within the skull. This occurs within the intracranial space anywhere brain tissue can move or push against structures (such as the falx cerebri, tentorium cerebelli) or through openings (such as the foramen magnum). This is often due to conditions that increase intracranial pressure rapidly, such as traumatic brain injury, hemorrhage, brian tumors, cerebral edema, or severe ischemic stroke. Since cerebral herniation can lead to compression of vital brain structures, it can cause neurological deficits such as altered consciousness, abnormal pupil size/reactivity, motor weakness, abnormal posturing (decerebrate, decorticate), respiratory abnormalities, and if left untreated, can result in coma or death. Imaging studies with CT or MRI may reveal midline shift, compression of ventricles, displacement of brain structures, or signs of herniation, which can aid in the identification of the specific type of herniation and guiding urgent management to relieve intracranial pressure and prevent irreversible brain damage. 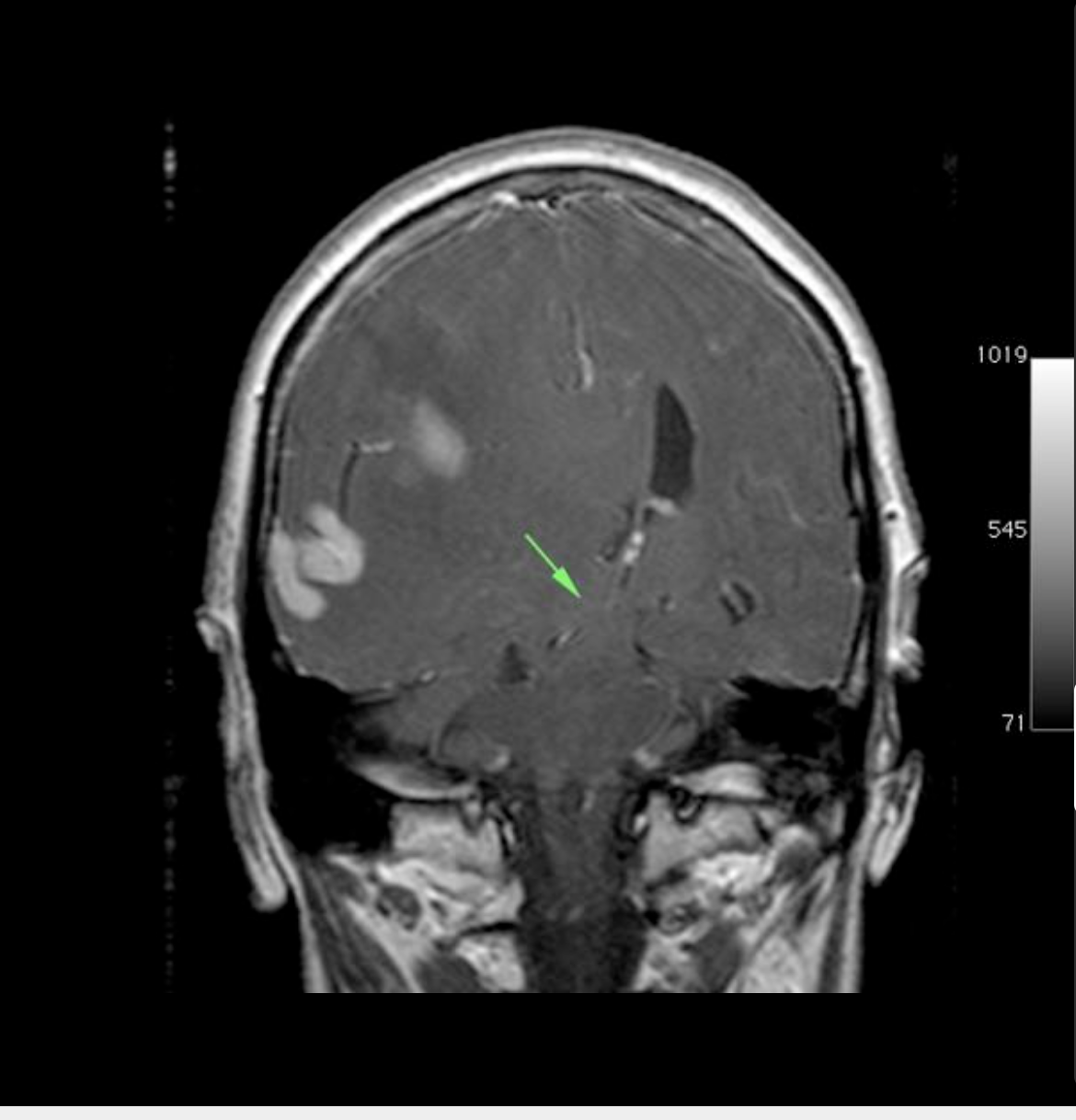
https://radiopaedia.org/cases/kernohan-phenomenon?lang=us
Hydrocephalus Hydrocephalus is a condition characterized by the abnormal accumulation of cerebrospinal fluid (CSF) within the ventricular system of the brain, leading to increased intracranial pressure. This can occur due to various factors, including obstruction of CSF flow within the brain (non-communicating hydrocephalus) or impaired CSF absorption outside the brain (communicating hydrocephalus). Causes for these may include congenital malformations, tumors, infections, hemorrhage, or complications related to developmental abnormalities. Symptoms may vary depending on the age of onset and the rate of fluid accumulation.
- Infants may present with a rapid increase in head size, bulging fontanelle, vomiting, irritability, poor feeding, and developmental delays.
- Adults and older children might experience headaches, nausea, visual disturbances, gait disturbances, and cognitive impairments.
Imaging with CT or MRI will reveal enlarged ventricles and increased CSF within the brain. Treatment often involves surgical intervention to divert or drain excess CSF, depending on the underlying cause and severity of the condition.
 https://thecommonvein.net/media/23063.jpg
https://thecommonvein.net/media/23063.jpgHydrocephalus Extraaxial Tumors Extraaxial tumors refer to tumors that develop outside the brain tissue but within the intracranial compartment, specifically in the spaces inside the skull surrounding the brain (extradural or subdural spaces) or in structures such as the meninges or cranial nerves. The most common extraaxial tumor arises from the meninges (meningiomas), but they can also arise from various other tissue types, including cranial nerves (schwannomas), and metastases from primary tumors elsewhere in the body. Symptoms can vary widely depending on the location and size of the tumor, and may include headaches, seizures, focal neurological deficits (weakness, sensory changes, etc), visual disturbances, changes in mental status, or other signs related to increased intracranial pressure. Imaging with MRI or CT may reveal the presence, location, size, and characteristics of the tumor. Approaches to treatment depend on the tumor type, location, and individual patient factors, and involve surgical resection, radiation therapy, chemotherapy, or a combination. 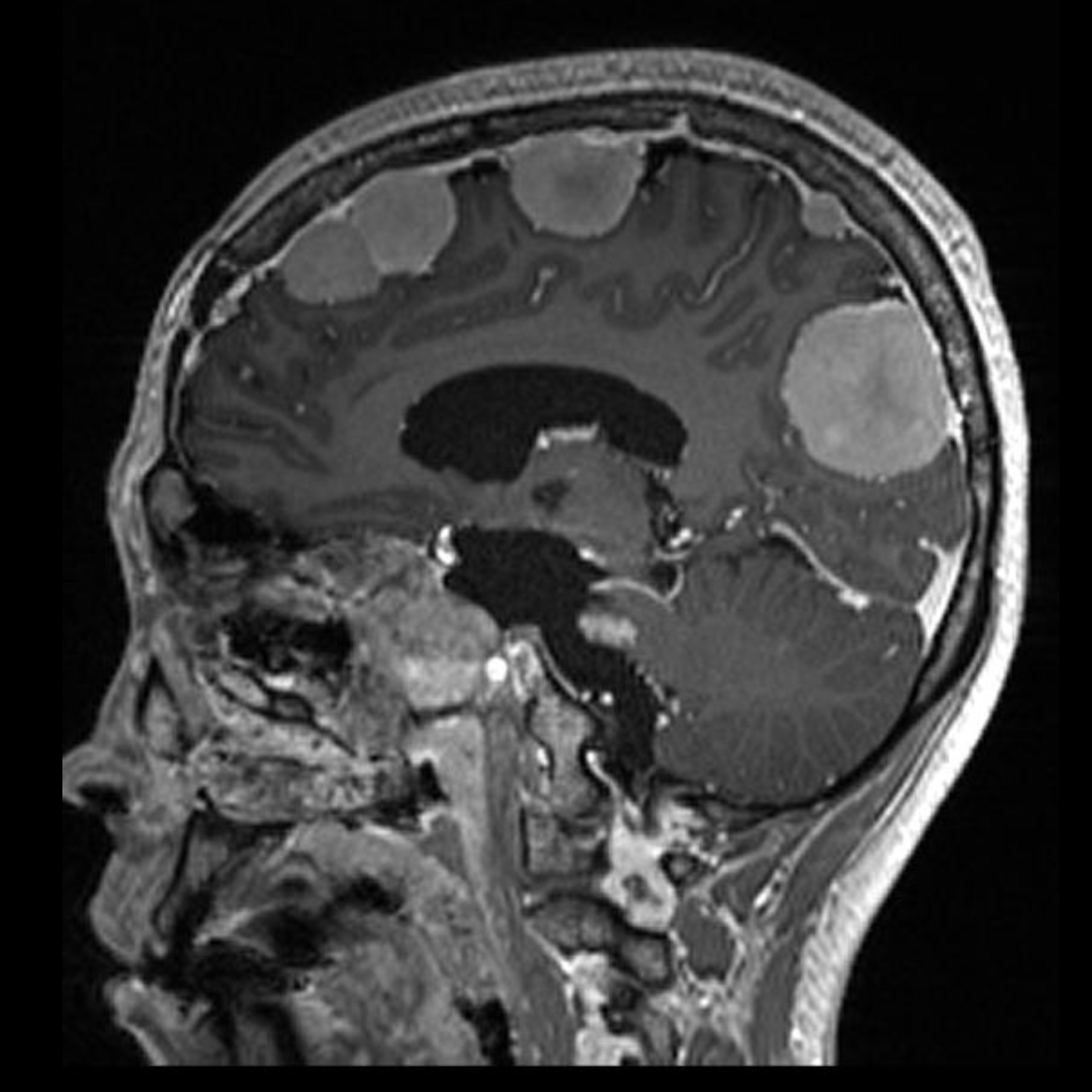
https://radiopaedia.org/cases/multiple-meningiomas-and-schwannomas-nf2?lang=us
Head and Neck Tumors Head and neck tumors refer to abnormal growths or masses that develop in the structures located in the head and neck region, including the oral cavity, throat, larynx, nose, sinuses, salivary glands, thyroid gland, and lymph nodes. They can arise from different tissue types, including squamous cells (squamous cell carcinomas), glandular cells (adenocarcinomas), lymphoid tissues (lymphomas), or other cell types. Risk factors for these tumors may include tobacco and alcohol use, human papillomavirus (HPV) infection, genetic factors, and environmental exposures. Symptoms vary depending on the location and type of tumor, but may include a lump/mass in the neck, changes in voice, difficulty swallowing, persistent sore throat, hoarseness, ear pain, nasal congestion, facial pain, or persistent coughing. Diagnosis involves a combination of imaging studies (CT, MRI, PET), biopsies, and other diagnostic procedures to determine the location, size, and nature of the tumor. Approaches to treatment depend on the tumor type, stage, and individual patient factors, and may include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of these modalities. Early detection and appropriate treatment can significantly impact outcomes for head and neck tumors. 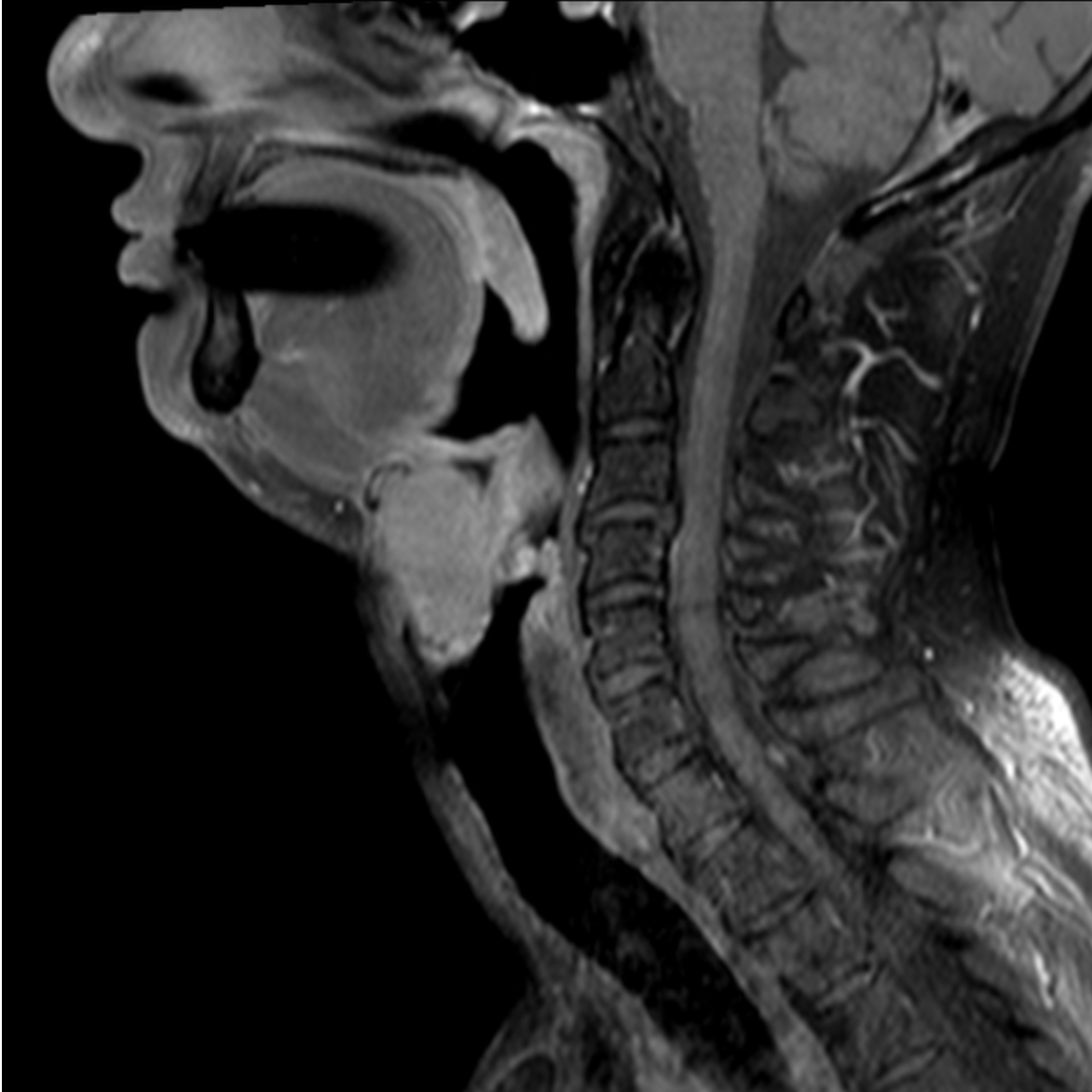 https://radiopaedia.org/cases/squamous-cell-carcinoma-of-larynx-with-transglottic-spread-t4?lang=us
https://radiopaedia.org/cases/squamous-cell-carcinoma-of-larynx-with-transglottic-spread-t4?lang=us
Intraaxial Tumors Intraaxial tumors are abnormal growths or masses that develop within the tissue of the brain itself, rather than in the spaces or coverings surrounding the brain. The most common intraaxial tumor is the astrocytoma arising from glial cells, but can also arise from various other tissue types including other glial cells (oligodendrogliomas, ependymomas), neuronal cells (gangliogliomas), or other specialized cells. The specific cause of intraaxial tumors is often unclear, though certain genetic factors, exposure to radiation, or environmental influences may contribute. Symptoms can vary depending on the location, size, and rate of growth of the tumor, and may include headaches, seizures, changes in mental status, focal neurological deficits (weakness, numbness, speech difficulties, vision changes), and altered cognitive functions. Imaging with MRI or CT may reveal the presence, size, location, and characteristics of the tumor within the brain tissue. Approaches to treatment depend on the type of tumor, its location, and its grade/aggressiveness, and may include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of these modalities. 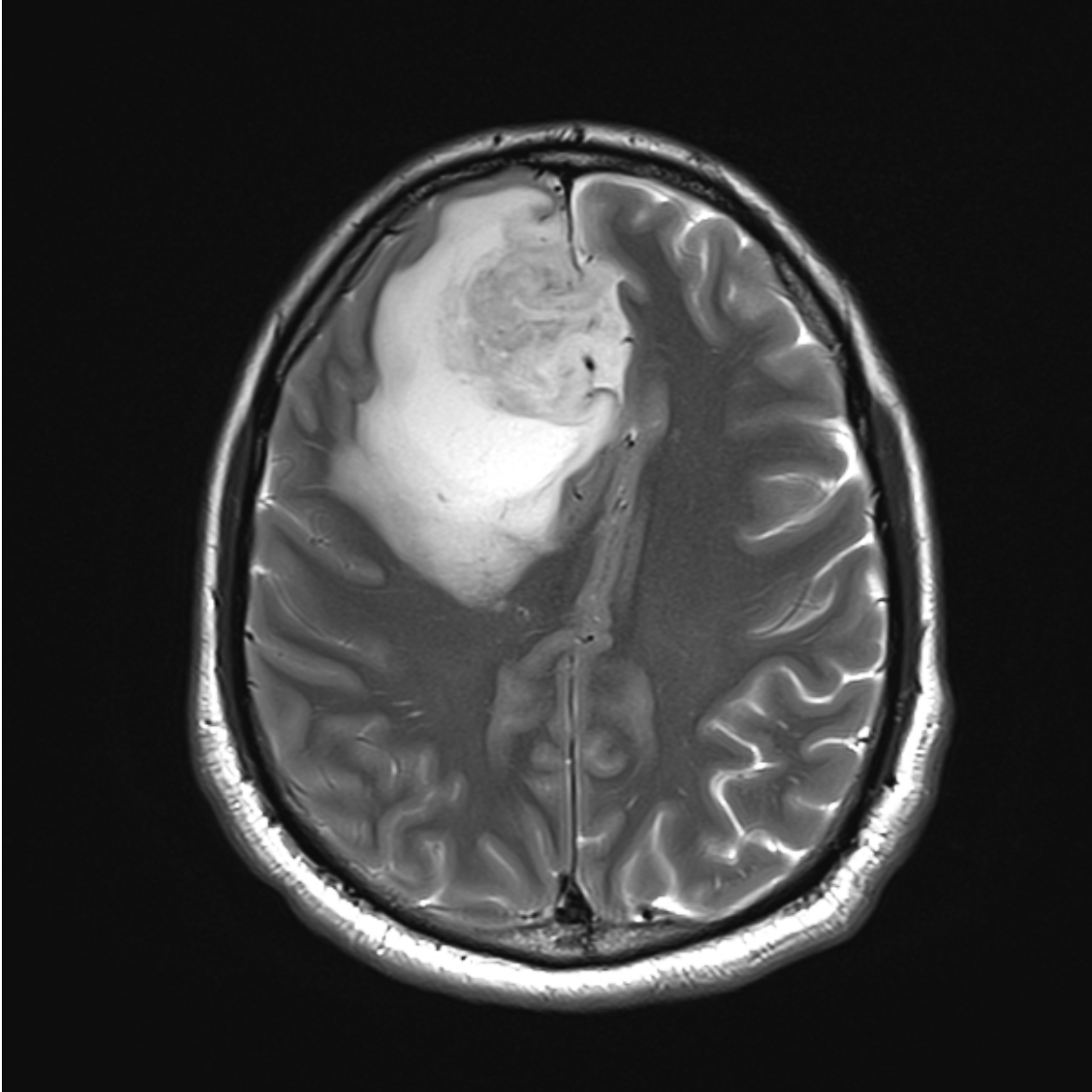
Brain Metastases Brain metastases refer to the spread of cancer cells from a primary tumor located elsewhere in the body to the brain, forming secondary tumors or metastatic lesions within the brain tissue. This is often caused by cancer cells breaking away from the primary tumor and traveling via the bloodstream or lymphatic system to the brain to establish secondary tumors. Common primary cancer sites that may metastasize to the brian include the lungs, breasts, skin (melanoma), kidneys, and colon, among others. Symptoms can vary widely based on the number, size, and location of the brain metastases, and may include headaches, seizures, changes in mental status, focal neurological deficits (weakness, sensory changes, speech difficulties), balance problems, and personality changes. Imaging with MRI or CT may reveal the presence, number, size, and locations of the metastatic lesions within the brain. Approaches to treatment depend on the type of primary cancer, extent of metastases, and the patient’s overall health, and may include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of these modalities. 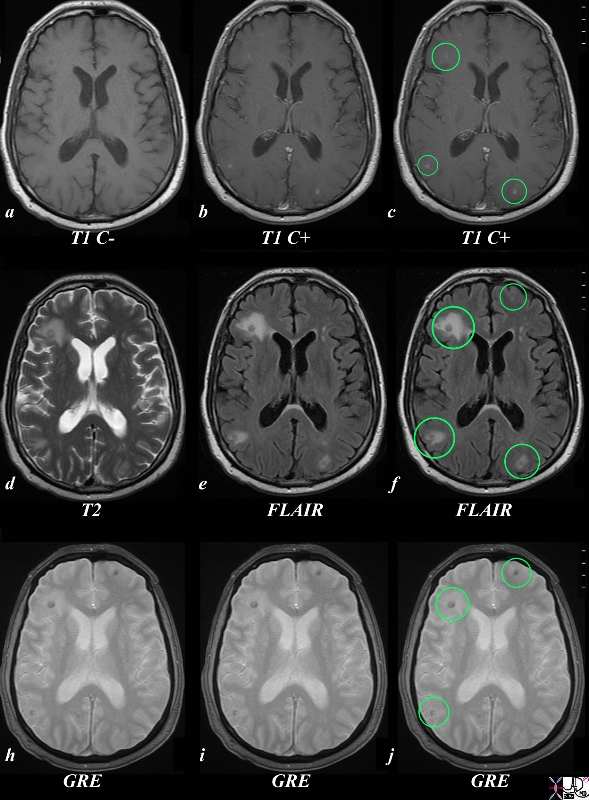 https://www.thecommonvein.net/media/89546c.8s.jpg
https://www.thecommonvein.net/media/89546c.8s.jpgBrain Metastases Malignant Brain Mass A malignant brain mass refers to an abnormal and cancerous growth within the brain tissue that exhibits aggressive and invasive behavior, potentially spreading to other parts of the brain or the central nervous system. They typically originate from within the brain itself (primary brain tumors) and are composed of rapidly dividing abnormal cells. The most common malignant brain mass arises from glial cells (gliomas), but they can also arise from various other tissue types, including neuronal cells or other specialized cells within the brain. Symptoms can vary based on the location, size, and aggressiveness of the tumor, and may include persistent headaches, seizures, changes in mental status, focal neurological deficits (weakness, sensory changes, speech difficulties), altered cognitive functions, and personality changes. Imaging with MRI or CT may reveal the presence, location, size, and characteristics of the malignant brain mass. Approaches to treatment depend on the type of tumor, its grade or aggressiveness, its location, and the patient’s overall health, and may include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of these modalities to control the tumor and manage symptoms. 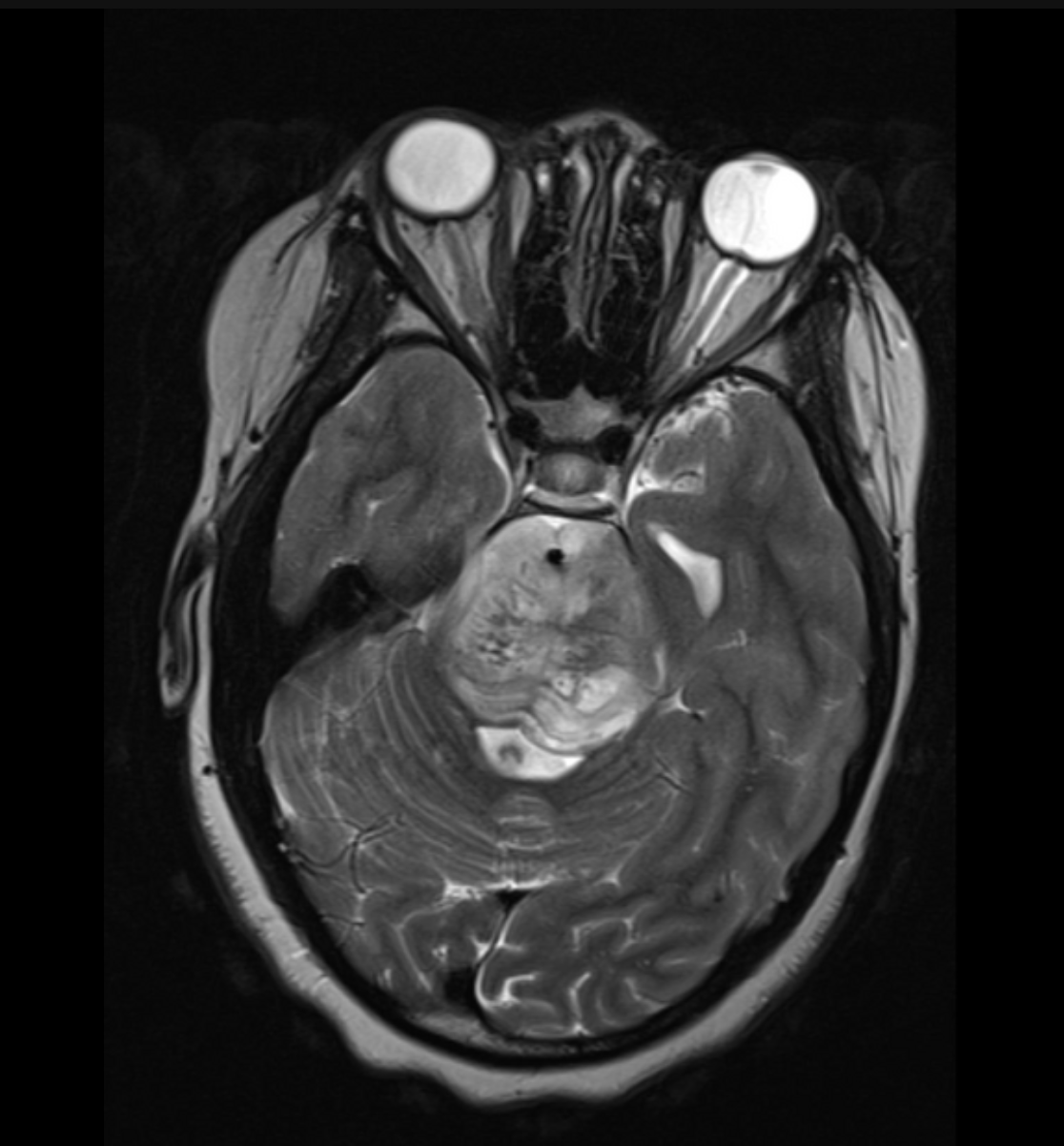 https://radiopaedia.org/cases/brainstem-glioma-5?lang=us
https://radiopaedia.org/cases/brainstem-glioma-5?lang=usBenign Brain Mass A benign brain mass refers to an abnormal growth or tumor within the brain tissue that is non-cancerous and generally does not invade nearby tissues or spread to other parts of the body. They typically originate from within the brain itself (primary brain tumors) and consist of cells that grow slowly and do not have the capacity to metastasize. The most common benign brain mass is the meningioma, but they can also include pituitary adenomas or certain types of gliomas with lower-grade characteristics. Symptoms can vary depending on the location, size, and effects of the mass on surrounding structures, and may include headaches, seizures, focal neurological deficits (weakness, sensory changes, visual disturbances), altered mental status, while some benign brain masses may remain asymptomatic and are only incidentally discovered. Imaging with MRI or CT may reveal the presence, location, size, and characteristics of the benign brain mass. Approaches to treatment depend on the type of tumor, its location, and the patient’s overall health, and may include observation, surgical removal, radiation therapy, or other interventions aimed at managing symptoms or preventing complications associated with the mass. 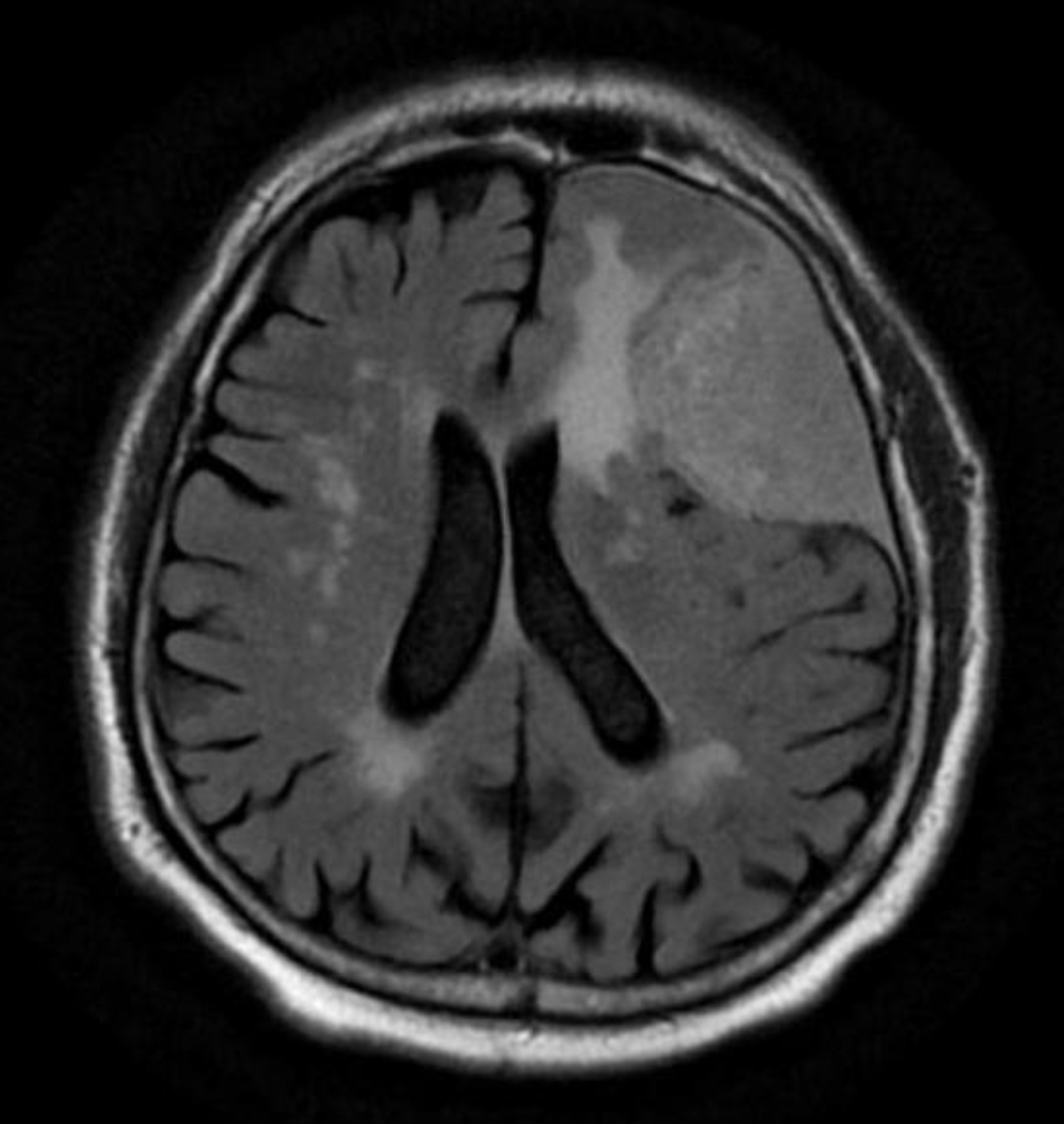 https://radiopaedia.org/cases/meningioma-39?lang=us
https://radiopaedia.org/cases/meningioma-39?lang=usIncreased Intracranial Pressure Increased intracranial pressure (ICP) refers to elevated pressure within the skull, potentially due to various pathological conditions affecting the brain. This occurs within the cranial cavity and involves the brain tissue, cerebrospinal fluid (CSF), and blood. Increased ICP can result from various conditions such as traumatic brain injury, intracranial hemorrhage, brain tumors, hydrocephalus, cerebral edema, or infections affecting the brain. Symptoms may include headaches that worsen with changes in body position of Valsalva maneuvers, nausea, vomiting (especially without associated gastrointestinal symptoms), altered mental status (ranging from confusion to coma), changes in vision (blurry/double vision), focal neurological deficits (weakness in limbs or facial muscles), seizures, papilledema (swelling of the optic disc). Imaging with CT or MRI may be performed to confirm the cause of increased ICP, and may reveal the phenomenon of mass-effect from the increased pressure, which includes effacement of the ventricles/basal cisterns/other CSF spaces, and in severe cases, loss of grey-white matter differentiation and/or brain herniation. However, diagnosis of increased ICP is mostly done clinically, through neurological assessment, evaluation of vital signs, consideration of the patient’s symptoms, and potentially lumbar puncture to determine opening pressure. Approaches to management aims to reduce ICP as well as alleviate the underlying cause, and may include medications to control cerebral edema, surgical interventions to relieve pressure (draining fluid, removing mass), and monitoring in an intensive care setting to prevent complications associated with elevated ICP. 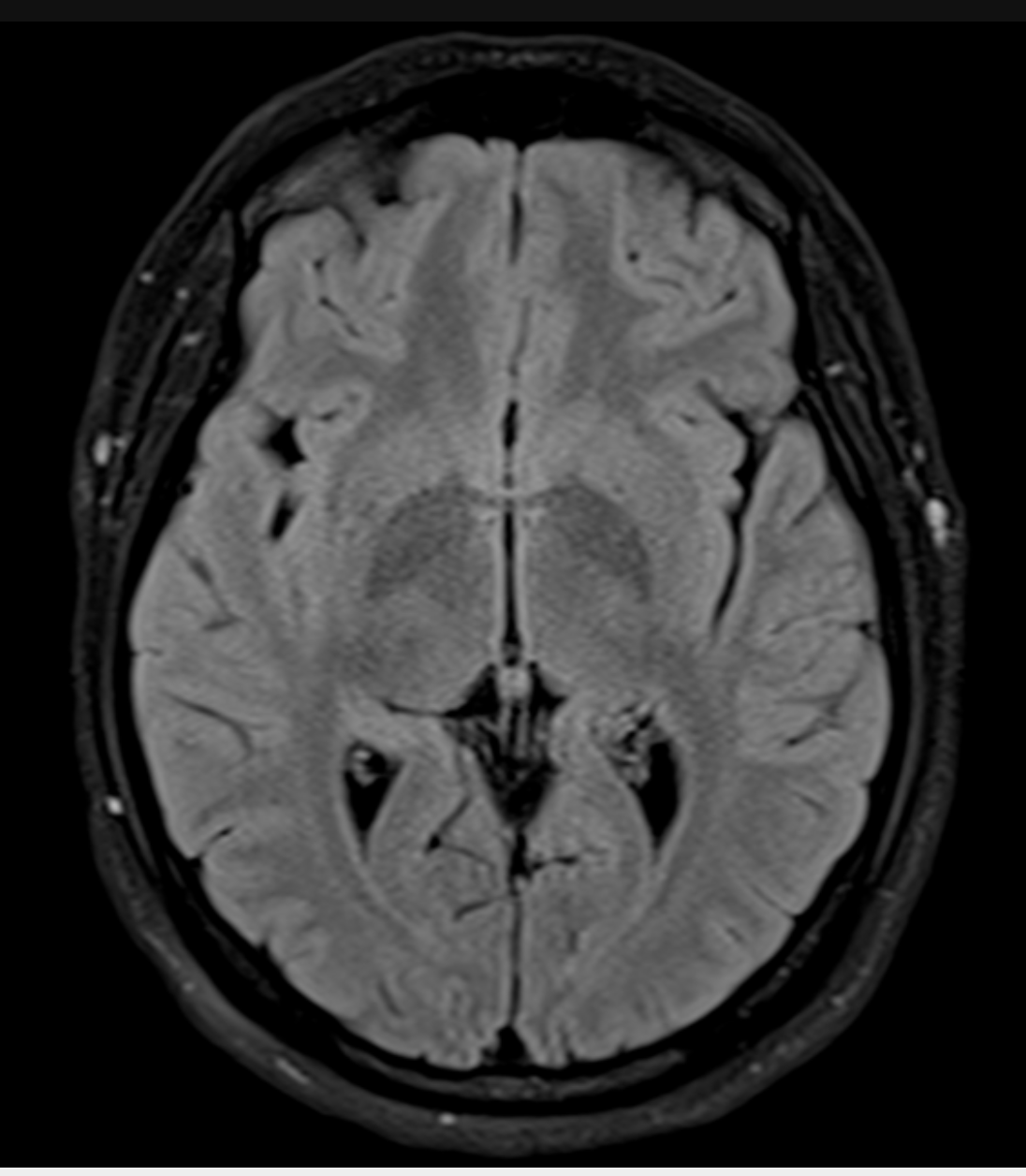 https://radiopaedia.org/cases/idiopathic-intracranial-hypertension-44?lang=us
https://radiopaedia.org/cases/idiopathic-intracranial-hypertension-44?lang=usIschemic Stroke Ischemic stroke is a cerebrovascular event caused by sudden interruption or blockage of blood flow to a specific vascular territory of brain tissue, with the lack of oxygen and nutrients leading to tissue damage. This is predominantly caused by the occlusion of a blood vessel supplying the brain, often due to a blood clot formed within the vessel (thrombus) or a blood clot that travels from another location and lodges within the brain’s blood vessels (embolus). The type, location, and severity of symptoms depend on the affected area of the brain, and may include sudden onset of weakness or paralysis on one side of the body (hemiparesis), numbness, difficulty speaking or understanding speech (aphasia), vision changes, sudden severe headache, loss of coordination, and altered mental status. Imaging with CT or MRI may reveal areas of brain tissue affected by ischemia, and additional imaging with angiography or echocardiography may be performed to determine the cause of the stroke. Immediate treatment involves restoring blood flow to the brain, which may involve medications such as tissue plasminogen activator (tPA) to dissolve clots or mechanical thrombectomy to physically remove the clot. Long-term management includes medications to prevent further clot formation, rehabilitation to regain lost function, lifestyle modifications, and addressing risk factors such as hypertension, diabetes, and high cholesterol to prevent recurrent strokes. 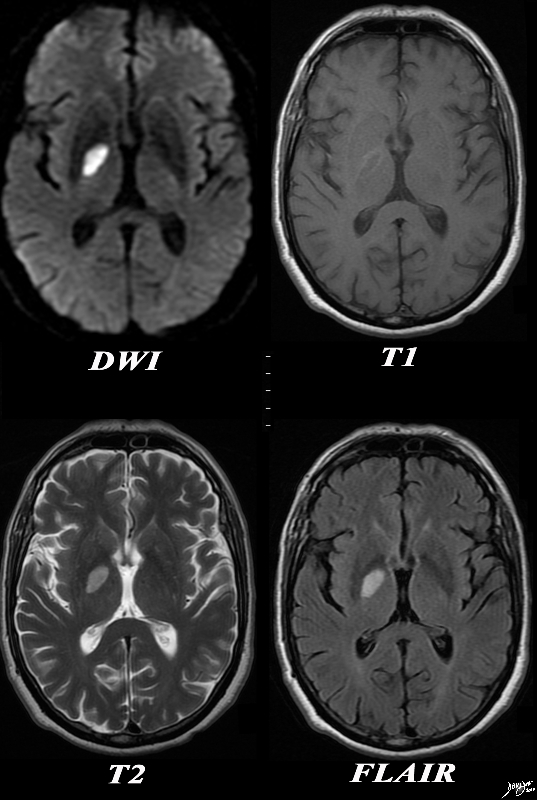 https://thecommonvein.net/media/89087c01.8s.jpg
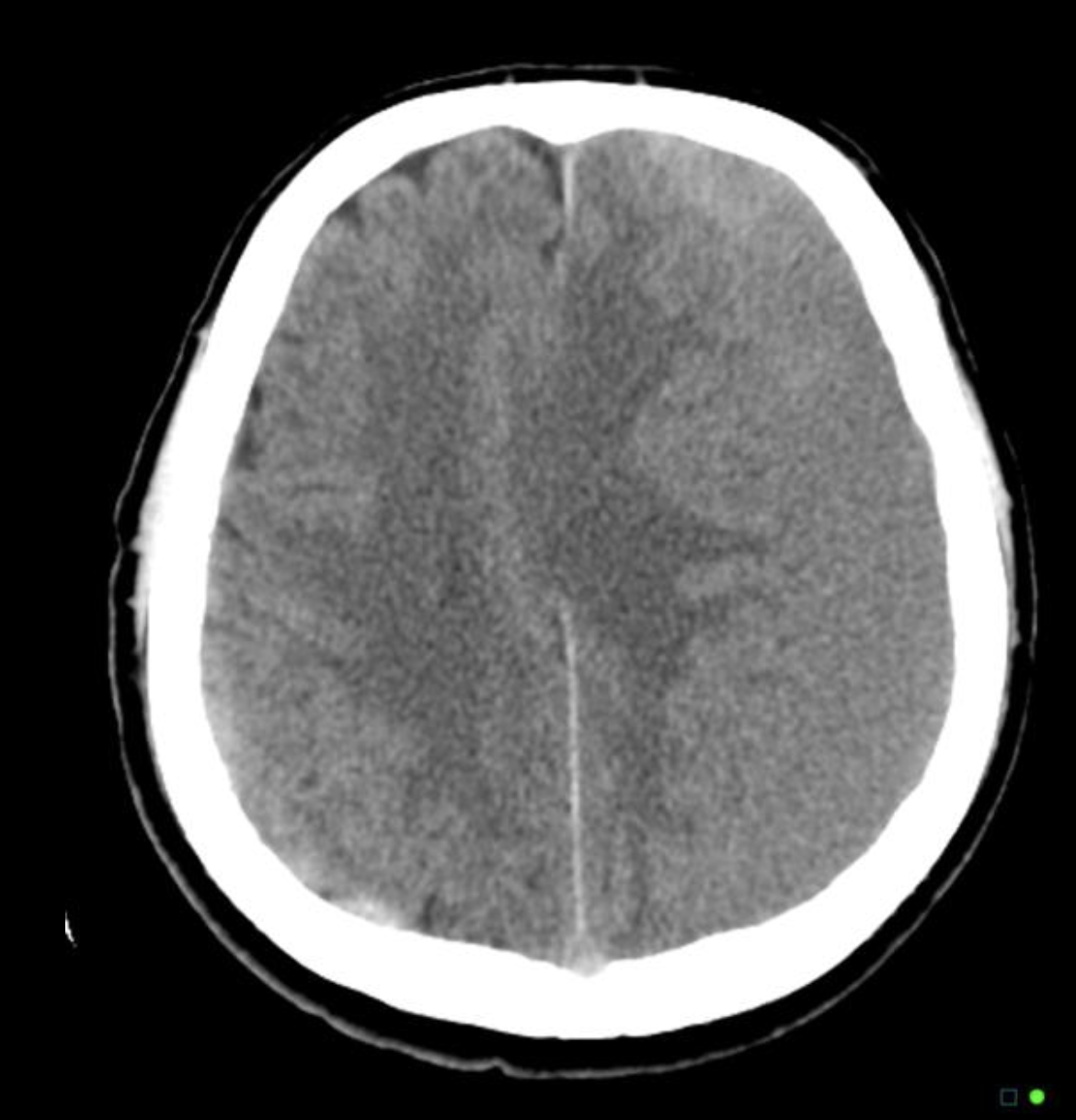
https://thecommonvein.net/media/89087c01.8s.jpgStroke Transient Ischemic Attack A transient ischemic attack (TIA), often referred to as a “mini-stroke”, is a temporary episode or brief period of neurological dysfunction caused by a temporary disruption of blood flow to a specific vascular territory of brain tissue. Similar to ischemic strokes, TIAs are caused by a temporary blockage of blood flow, often due to a blood clot (embolus or thrombus). However, the blockage in TIA is transient and resolves spontaneously, usually within a few minutes to a few hours. Symptoms of a TIA are similar to those of an ischemic stroke but tend to be transient and reversible, and may include sudden weakness or numbness on one side of the body, temporary loss of vision in one/both eyes, slurred speech, difficulty speaking or understanding, or temporary difficulty with balance or coordination. Imaging with CT or MRI may be performed to rule out an ongoing stroke or to determine the underlying cause, but diagnosis of TIA is mostly based on the presence of transient neurological symptoms that resolve within 24 hours. Immediate medical attention is crucial to evaluate and manage a TIA, and treatment involves identifying and managing underlying risk factors to prevent a subsequent stroke, which may include lifestyle modifications (diet, exercise, smoking cessation), and medications to control blood pressure, cholesterol levels, and blood-thinning agents to prevent clot formation. 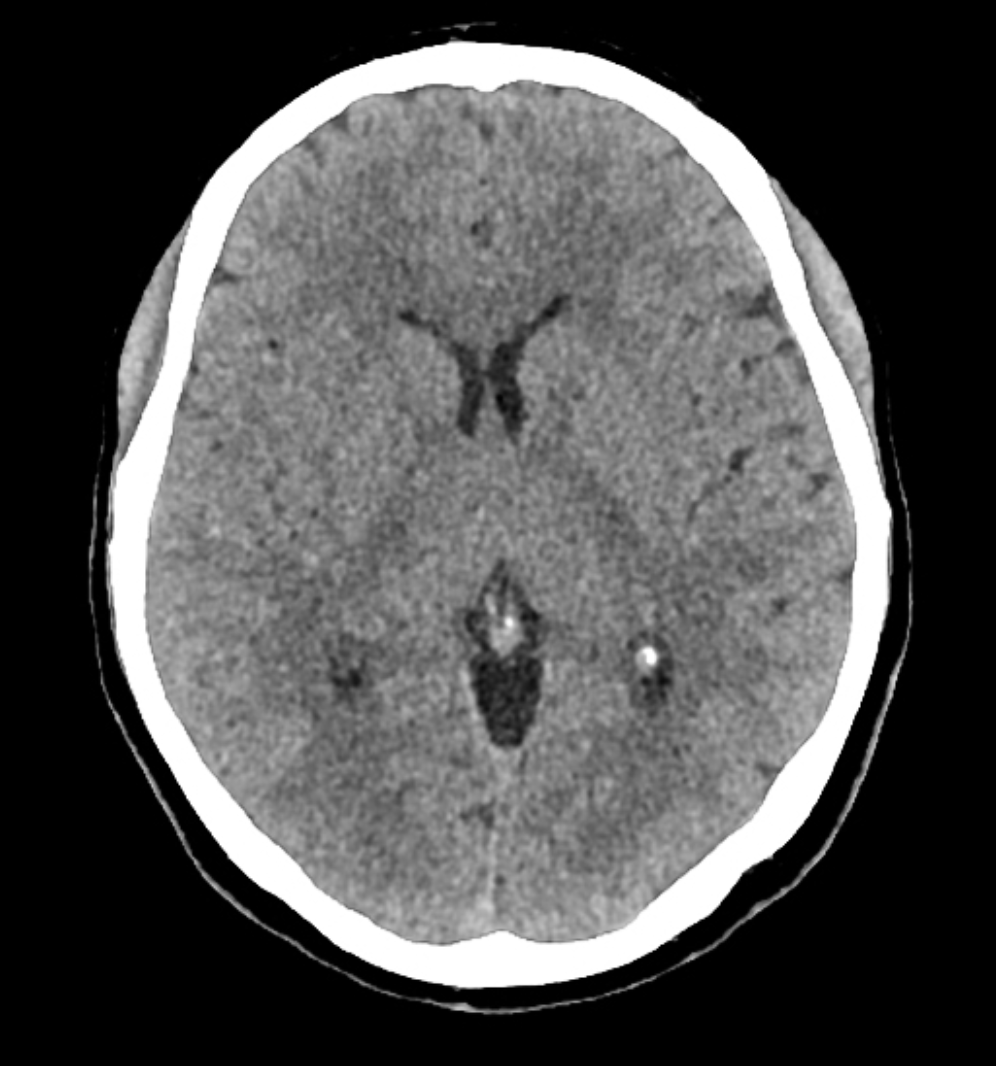 ^Normal brain CT indicating no ischemic stroke
^Normal brain CT indicating no ischemic stroke
Transient Ischemic Attack
Common chief complaints:
WF NEURO INDEX
-
Modality
-
CT
- IF CT Non – Contrast
IF CT with Contrast
IF CTA
IF CT Density Measurement Water
IF CT Density Measurement Soft Tissue - IF CT Density measurement Air
- IF CT Density measurement Fat
-
- MRI
-
- T1
- T1 with contrast
- T2
- DWI
- T1
- MRA
-
-
Findings
abscess cerebral TCVabscess paraspinalage related changes TCVaneurysm cerebral TCVcompression spinal cord image 102190c05L.8sdementia (atrophy)diffuse axonal injuryhemorrhage hematoma subduralhemorrhage hematoma epiduralhemorrhage hematoma Intracerebralhemorrhage hematoma Isodense subduralshemorrhage hematoma subarachnoid hemorrhagehemorrhage hematomas of different ages in nonaccidental trauma (NaT)herniation cerebralhydrocephalusmass extraaxial tumorsmass head and neck tumorsmass Intraaxial tumorsmass metastasesmass malignantmass benignsigns increased intracranial pressure -
Diseases
- Demyelinating diseases
Discitis/Osteomyelitis
Meningitis
Sinusitis
Stroke Hemorrhagic
Stroke Hemorrhagic
Trauma Brain
Trauma Cervical spine
Trauma Facial trauma
- Demyelinating diseases
-
What Next? ACR Appropriateness Criteria
- AIDS in the CNS (MR vs PET vs thallium)
CNS tumor recurrence vs radiation necrosis (MR vs PET vs thallium)
Criteria for performing CT prior to lumbar puncture
Dementia
Dizziness
Encephalitis
Facial trauma (radiographs vs CT)
Headache (CT vs MR vs none)
Meningitis
Metastatic disease to CNS (CT vs MRI, contrast)
MRA negative patient with subarachnoid hemorrhage
Multiple sclerosis
Paranasal sinus disease (radiographs vs CT vs MR vs none)
Proven non-traumatic intracerebral hemorrhage (CTA vs MRA vs angio)
Seizures
Spinal trauma
Stroke – early and late (CT vs MR vs angio)
Stroke patient with evidence of hemorrhage
Stroke patient without evidence of hemorrhage (timing) with or without CT evidence of infarct
Suspected SAH (CTvs MRI vs angio)
Suspected stroke patient (CT vs MRI)
TIAs
When conventional neuroangiography is indicated
When myelography is indicated vs MR
When to request spine CT vs MR vs radiographs
- AIDS in the CNS (MR vs PET vs thallium)